What are you planning to do during surgery?
A hip arthroscopy means “looking inside a hip joint”, which is only the first part of the procedure. Surgeons use cues from the history of the injury, the pre-operative physical examination, the X-rays, and the MRI to formulate a provisional plan for surgery. Obviously, visualizing the hip joint with the camera gives additional information, which can change the plan. Most patients with labral tears of the hip have a bony, structural cause for the tear. Ask your surgeon if he/she plans to address the cause of the tear, and how they plan to accomplish that. The recent research clearly shows benefit of labral repair vs. debridement. Ask your surgeon what he/she plans to do with the labral tear. The only way to REPAIR a labral tear is with suture (surgical string), usually also with bony anchors (see pictures below). Otherwise, the procedure is a debridement (trimming away some labrum around the tear site).
How many procedures have you performed? How many did you do last year?
There is no set minimal number of hip arthroscopies a surgeon needs to do before they are technically proficient. However, with a more experienced surgeon, the complication risk does go down and the chance of success of the operation improves. In a study I performed in 2010, looking at both novice and experienced surgeons, it took a minimum of 50 hip arthroscopies per year before a surgeon even plannedFAI surgery in a similar way to a surgeon who performs more than 200 hip arthroscopies per year.
Ask what percentage of cases involve FAI osteoplasty (reshaping the bone of the socket side (acetabulum), the ball side (femoral neck), or both. Also ask what percentage of cases involve suture anchor labral repair. In younger patients, the percentage of cases where I perform FAI osteoplasty and labral repair for a symptomatic labral tear is greater than 95%. It is extremely rare for me to perform a labral debridement alone.
What are the complications and chances of success of the procedure?
With advances in hip arthroscopic techniques and instrumentation, the complication rates are lower, but unfortunately they are not zero. Ask your surgeon about his/her complication risks. Has their patient ever had a fracture or dislocation? Has any patient been worse following the procedure? What percentage of their patients get back to competitive sports, at the same level they were at before they had hip pain?
What is the recovery time?
Surgeons may have different protocols based what procedure is actually performed during hip arthroscopy. In general, if there is significant gliding cartilage damage, the surgeon may have to perform microfracture (poking holes in areas of bare bone, trying to get repair cartilage to grow in the defect). Microfracture recovery can mean being on crutches for an extended period of time (4-8 weeks). If the procedure involves FAI osteoplasty and labral repair, the time on crutches is significantly lessened. In my patients, they typically are on crutches until they can walk comfortably without a noticeable limp, which is usually between 2 days and 2 weeks after surgery.
Physical therapy is usually a part of the recovery process as well. My hip FAI rehabilitation protocol usually last between 8-10 weeks. Getting back to competitive sports depends of the specific activity, and can be between 3-6 months.
SUMMARY: Hip arthroscopy is a wonderful tool to improve patients’ lives. Patients should get as much information as possible before surgery, so they can make informed decisions regarding their care.
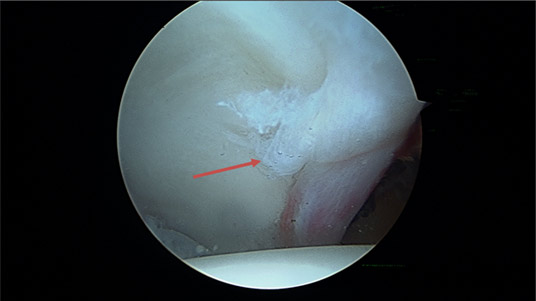
Above is a picture of a typical labral tear in a high level ballet dancer. The red arrow is pointing towards the tear.
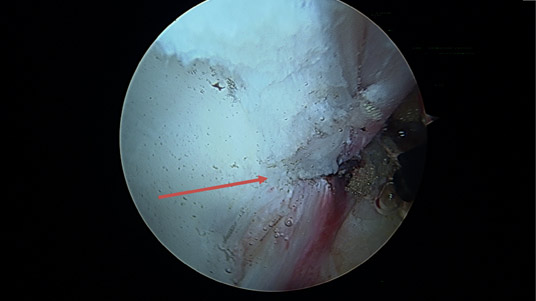
Here is the same view after a suture anchor has been placed in the bone and tied around the labrum (red arrow)
